September 23, 2025
Executive Summary
In today's volatile global trade environment, smart supply chain strategies are essential for medical device manufacturers impacted by tariffs and shifting trade policies. These strategies enhance supply chain resilience, supporting operational continuity and long-term stability as well as cost efficiencies and product availability. By maintaining expectations when realigning medical device supply chains, manufacturers can minimize expensive delays, legal risks, and market disruptions.
Exponent brings proven value to medical device manufacturers by combining deep regulatory knowledge with cross-disciplinary technical expertise to support rapid evidence-based decision-making, helping clients improve patient safety, secure market access, and support sustained commercial success amid evolving geopolitical and economic pressures.
How can manufacturers swiftly address and mitigate risks when onshoring or nearshoring materials, components, and processes for critical medical devices?
As tariffs and counter-tariffs create uncertainty across global supply chains, medical device manufacturers face heightened challenges in maintaining production continuity and patient safety while meeting complex regulatory requirements, including those set by the U.S. Food and Drug Administration and the EU Medical Device Regulation (MDR).
For producers of critical devices, such as stents, pacemakers, blood glucose monitors, and ventilators, adapting to supply chain shifts requires upholding safety and reliability throughout the product lifecycle. Failure to do so can result in delayed regulatory determinations, significant change management costs, increased patient risk, and potential legal exposure.
In this rapidly evolving economic landscape, companies that are onshoring or nearshoring medical device materials, components, and manufacturing processes can prioritize three key strategies:
- Rapid response capabilities to address disruptions and evolving regulatory expectations.
- Rigorous evaluation of vendors and partners to support quality, traceability, and compliance.
- Comparative risk and performance assessments to streamline approvals and validate safety across alternatives.
Drawing on our experience supporting major medical device manufacturers during the COVID-19 pandemic, Exponent offers a proven approach to reducing uncertainties when bringing products to market. Our methodology helps clients enhance supply chain stability, achieve cost efficiencies, and build long-term resilience — regardless of market fluctuations or macroeconomic pressures.
Why is rapid response so important?
When tariffs, shifting market forces, or global supply chain disruptions force medical device manufacturers to change vendors for essential materials or components on short notice, rapid response becomes critical to maintain regulatory compliance, market access, and uninterrupted patient care.
For example, in the case of a battery substitution in a pacemaker, even minor variations in battery chemistry, casing materials, or the internal assembly process can significantly impact the device's longevity, electrical performance, or electromagnetic compatibility — all of which are critical to patient safety and device reliability. Once a new battery is selected, manufacturers must not only validate equivalent performance through rigorous testing but also thoroughly document the changes and supporting data for regulatory authorities. Any gaps in this process can delay clearance or approval or introduce new safety risks.
Managing these transitions can be complex and time sensitive. For example, when replacing electronic components, manufacturers may need to evaluate thousands of potential alternatives. Conversely, in cases involving specialized sterilization techniques or polyethylene materials used in joint replacements, there may be only a handful of qualified global suppliers. This presents two distinct challenges: navigating an overwhelming number of options or competing intensely for limited resources with reduced negotiating flexibility.
In both scenarios, success hinges on executing a rigorous and expedited change management process. However, speed without rigor risks long-term compliance and safety liabilities. A truly effective rapid response requires a multifaceted approach.
- Alternative supplier identification and thorough vendor evaluations: A rapid evaluation will necessarily involve an investigation into the alternative supplier's documented quality system as well as the reality of their on-the-floor process controls. This means deploying appropriate technical experts for on-site audits to verify that manufacturing practices align with quality, reliability, and regulatory requirements.
- Robust risk and performance assessments: New components, materials, or processes introduce the potential for previously unidentified failure modes. A robust assessment can anticipate the potential for not only immediate functional failures, but also synergistic risks and latent failure modes introduced by new material interactions or subtle variations in process.
- Accelerated testing and validation protocols: With limited time and components, an optimized testing protocol can benefit manufacturers. Protocols can be strategically designed to create a high-impact test matrix that generates submission-ready evidence efficiently and without the need for repeat studies.
- Meticulous regulatory compliance documentation: Change and change control documentation under the stress of timelines has the potential to create additional long-term gaps. Ensuring the changes are planned, executed, and documented, even under time-sensitive circumstances, is critical to future product changes, iterations, and decisions.
Effectively managing these elements can help support a smooth transition with minimal risk to product safety, regulatory timelines, and patient outcomes.
Even a substitution that seems minor can have far-reaching implications for both device safety and regulatory compliance.
What are the benefits of evaluating (and re-evaluating) vendors?
As tariffs and broader economic pressures disrupt global supply chains, medical device manufacturers are increasingly compelled to explore new vendors or reconsider previously eliminated suppliers. These shifts demand more than just a logistical adjustment — they require a thorough technical validation process to confirm that potential suppliers can consistently meet the stringent quality, reliability, and regulatory requirements unique to medical devices. Without rigorous vetting, manufacturers can risk compromised product integrity, delayed market access, or failure to meet regulatory requirements.
Even with robust and proactive change control processes in place, every new vendor comes with new potential sources of failure and risk across the medical device product lifecycle. This is especially critical for components like coatings, which play essential roles in biocompatibility and patient outcomes. For example, drug-eluting coatings on stents and hydroxyapatite coatings on dental and orthopedic implants are vital for promoting tissue integration, accelerating healing, and reducing the risk of rejection. Any variation in coating composition or application technique due to a supplier change must be carefully assessed. To support vendor selection, manufacturers can thoroughly evaluate:
- Quality management certifications (e.g., ISO 13485)
- Approaches to process validation and risk management, including the use of process failure mode and effects analysis (PFMEA)
- Technical validation protocols, with a focus on meeting requirements for biocompatibility, durability, and performance consistency
Attention should also be given to a vendor's ability to control and quantify particle generation, a critical safety factor with implications for biocompatibility and regulatory compliance. By examining the standardization of test equipment and analytical methods, manufacturers can confirm that the vendor meets both clinical safety expectations and regulatory standards, while also supporting the business imperative to adapt to tariff-driven or cost-related supply chain changes — without compromising patient safety or product quality.
How can comparative assessments demonstrate regulatory equivalence?
When changes in materials or component vendors result in substitutions with even slightly different characteristics or modified manufacturing processes, conducting comparative assessments will be required to demonstrate equivalence, safety, and reliability to regulatory authorities in the U.S., EU, and other global markets. By rigorously comparing new materials or components to those previously approved — through systematic physical, chemical, and performance testing and analysis — manufacturers can generate objective evidence that the substitution maintains the device's intended function without introducing new risks.
Even a substitution that seems minor can have far-reaching implications for both device safety and regulatory compliance. Consider the example of nearshoring a single capacitor within a much larger chip used in an implanted heart monitoring device. While a brief comparative analysis might confirm that the new component delivers equivalent electrical performance (such as current output and stability), true equivalence extends beyond primary functional specifications to encompass the full risk profile of the device in its intended clinical use environment.

A comprehensive risk assessment may uncover less obvious but critical factors. For instance, a subtle change in a capacitor's trace materials, while electrically insignificant, could alter the device's MRI compatibility, introducing patient risks from induced heating, image artifacts, or unintended stimulation. This type of overlooked second-order effect is often what differentiates a successful component substitution from one that leads to regulatory delays or potential post-market incidents.
By deploying teams of electrical, biomedical, mechanical, and chemical engineers, along with other domain specialists with extensive regulatory and industry experience, Exponent helps manufacturers identify, interpret, and test in accordance with relevant standards. Leveraging our extensive history in failure analysis, our experts can close gaps in overlooked yet essential safety elements, confirming that they are systematically evaluated and incorporated into change assessments that can significantly impact the success of regulatory submissions.
Comparative analyses may include:
- Rapid side-by-side bench testing
- Biocompatibility assessments
- Accelerated aging studies, where applicable
When clearly documented and scientifically justified, these evaluations can fulfill the EU MDR's equivalent demonstration requirements and align with FDA expectations for device modifications. More importantly, this approach reassures regulators, clinicians, and patients that product safety, performance, and reliability are maintained — despite necessary adjustments in supply chain or vendor relationships.
Putting it together: rigorous risk assessments and technical expertise
In today's rapidly evolving global trade environment, medical device manufacturers must navigate economic and political uncertainty while proactively mitigating product and organizational risk. Achieving this balance requires leveraging cross-disciplinary expertise — including deep technical knowledge and regulatory insight — to make informed decisions that uphold both compliance and innovation.
Whether preparing for new regulatory submissions, responding to supply chain disruptions, or managing material, component, or process substitutions, a structured approach is indispensable. Tools such as comparative assessments are critical for demonstrating device equivalency and maintaining regulatory compliance. Equally important is the systematic identification, evaluation, and mitigation of new or altered failure modes introduced by these changes.
To minimize risk and promote continued device reliability and safety, manufacturers can deploy established analytical techniques like failure mode and effects analysis (FMEA) and finite element analysis (FEA). These tools help identify potential vulnerabilities and guide the integration of technical findings into comprehensive risk management and regulatory compliance strategies.
As macroeconomic volatility increases and legal liabilities escalate, the ability to assess, validate, and de-risk substitutions is increasingly critical. This process not only helps safeguard patient safety but also strengthens market differentiation and supports sustainable commercial success in a competitive and complex global landscape.
Frequently Asked Questions
What Can We Help You Solve?
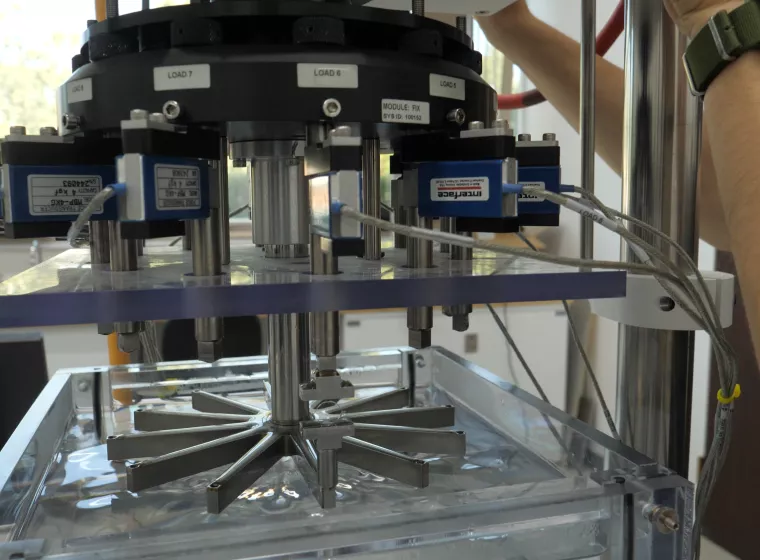
Exponent's multidisciplinary teams of biomedical engineers, polymer scientists, biostatisticians, and regulatory experts help medical device manufacturers navigate supply chain disruptions and materials, component, and processing substitutions. Our state-of-the-art biomedical laboratories and computational modeling capabilities enable our experts to perform advanced testing and failure analysis throughout the total product lifecycle.
Medical Device Evaluation
Sophisticated medical device evaluations for a vast array of applications.

Regulatory Compliance for Medical Products
Experienced regulatory support for medical devices, pharmaceuticals, and combination products.

Biomedical Engineering Laboratories
Expert biomedical laboratory services, delivering evidence-based answers for your most complex challenges.

Medical Device Design & Development Support
Crucial medical device design and development analyses to empower your decision-making.

Biomedical Expertise for Therapeutic Areas
Multidisciplinary insights for a range of therapeutic product development challenges.

Battery Safety & Risk Management for Medical Devices
Unmatched technical support, guidance, and insights for batteries in wearable and implantable medical devices.





