February 16, 2023

Understanding the impact of human factors on patient adherence to digital health technologies
Digital health solutions have the potential to transform healthcare, but successfully integrating these tools into research and patient care isn't as straightforward as disseminating devices and waiting for results to roll in. While digital health innovations are advancing quickly to meet rapidly evolving healthcare needs, attention up to this point has largely been focused on the accuracy and reliability of the data being collected — without as much consideration for how patients view these new technologies or where gaps in use may be surfacing
A patient-centric view
We're only at the beginning, but digital health technologies already show enormous potential to drive improvements in patient outcomes. Digital health solutions can, for example, help measure outcomes after a medical intervention, monitor adherence with a treatment plan or pharmacological therapy, or facilitate additional remote care and treatment through telehealth or reporting apps.
For these reasons, barriers that impact user adoption or adherence can have significant impacts on the value-add of the technologies themselves, including the quality of the data acquired, the validity and reliability of real-world evidence, the patient journey, and even health equity.
Using a human factors approach to evaluate barriers to patient adoption and adherence is essential to enabling sustainable, longitudinal use of innovative digital health solutions — and generating the insights needed to help guide the development of future healthcare innovation.
Taking a human factors approach means positioning the patient at the center of the technological solution, including its choice and implementation. Examples will encompass evaluating patient behaviors, the intended use of the device as well as how easy it is to use, and other accessibility, mobility, and demographic variables. Striking the right balance among these factors can reap benefits for both patients and providers, as strong adherence to a digital health technology promotes effective and informed clinical decision-making, with direct implications for patients' overall health and well-being.
Human factors: a vital piece of the digital health technologies puzzle
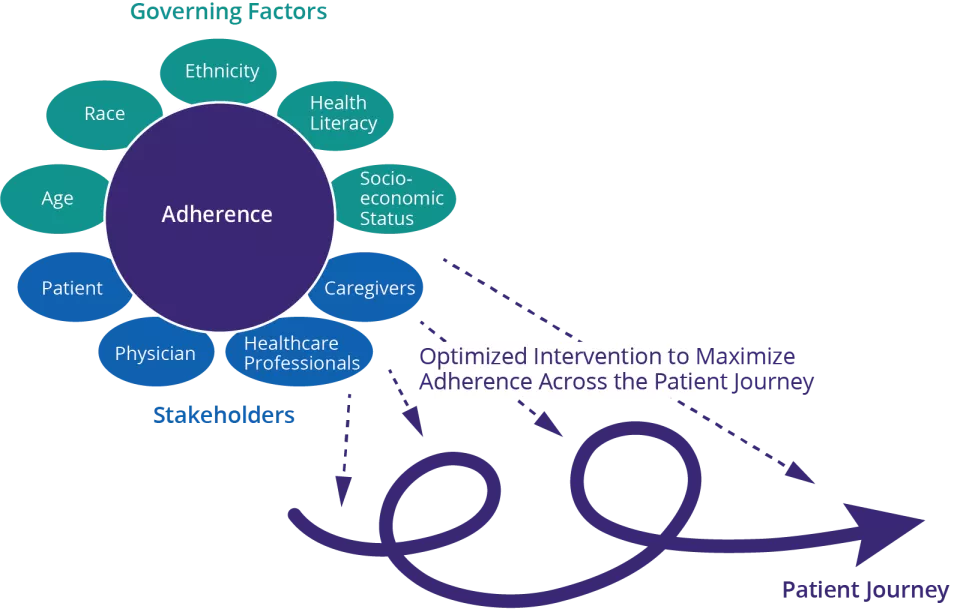
Extensive scientific literature has been published on patient adherence, and while no single intervention strategy can guarantee adherence among everyone, tailoring technological interventions to the unique characteristics of patients, their disease conditions, prescribed treatments, and social context is critical to success.
Building on existing research, human factors experts are now playing an important role in monitoring and enhancing patient adherence to digital health solutions by considering additional components of the human-technology interface.
A study published by the World Health Organization in December 2022 found that populations across Europe do not leverage digital health technologies equitably.
Some examples of these components include assessing usability aspects before a digital health technology is selected; monitoring adherence to the technology throughout the patient journey; and focusing on detecting non-adherence early by analyzing patient-generated health data so that timely interventions can be triggered as needed.
Evaluating patient adherence to digital health tools can also help stakeholders increase Diversity, Equity & Inclusion (DEI) efforts in healthcare, such as expanding a given patient population and augmenting the diversity of the data collected.
For example, a study published by the World Health Organization in December 2022 found that populations across Europe do not leverage digital health technologies equitably, with ethnic minorities, older populations, non-urban dwellers, and patients with poor health accessing digital tools less than those who are younger, white, educated, and living in urban areas. Rather than a limitation on implementation, however, research such as this can support human factors experts in understanding specific barriers to use and selecting or developing technologies that help overcome them.
The right digital health technology for the right patient population
Choosing the right technology solution must be driven by more than the information a healthcare provider typically captures. Rather, life sciences and pharmaceutical companies can increase the probability of success by anticipating obstacles based on the target patient population and intended use-case. For example, patients with rheumatoid arthritis may reject using a particular wrist-based digital technology if they are unable to fasten the device clasp; elderly patients who are tech-averse may find some interfaces confusing; and patients in certain geographical areas or socioeconomic groups may be unable to use a tool that requires Wi-Fi access or lengthy charging times.
Some factors to consider in selecting the right digital health technology include:
- Data accuracy, reliability, and availability
- Device connectivity and syncing
- Data storage capacity and buffering
- Battery life and charging requirements
- Device and metric maturity
- API/SDK availability
- Device and data security
- Wear location options and restriction
- Use options (apps, survey links, push notifications, etc.)
Likewise, on the tech side, companies developing digital healthcare tools can gain valuable insights by leveraging human factors expertise to assess patient adherence challenges and opportunities from the outset. User experience concepts typically focus on human-centered design and function and are often screened after a prototype is launched. Human factors analyses in the ideation phase enable developers to incorporate key patient adherence considerations into their digital health technology roadmaps from the start of the product lifecycle.
A working digital health adherence framework
A strategic framework can support stakeholders in operationalizing, monitoring, and evaluating human factors-related outcomes at each stage of the digital solution pathway. This framework can support developing direct recommendations or implementing novel strategies that enhance both acute and longitudinal patient adherence, such as the following:

Mapping the patient population
Selecting a digital technology typically begins with an analysis of the target patient population to understand the group's needs, anticipated operating environments, prior experience with the technology, and characteristics including gender, age, education, culture and ethnicity, physical and cognitive abilities, language, and health literacy.
Implementing a patient-centered approach when selecting a digital technology solution additionally promotes accommodating patient needs and their potential challenges, enabling user understanding and integration, and ultimately improving patient adherence to the technology from the outset. Early insights into the target patient population's needs coupled with knowledge of the digital technology's capabilities and limitations afford an objective and holistic approach to determining and deploying the optimal solution.

Prevention, intervention & remediation
Collecting and evaluating multiple patient-centric data streams is important during and after deployment of a digital solution to monitor and remedy (where appropriate) patient adherence to the technology in question.
Patient interviews, surveys, and focus groups, for example, can help identify challenges and inform real-time approaches to encourage improved adherence throughout the introduction, deployment, and utilization of a digital health tool. These approaches include patient engagement in decision-making around what and how the technology will be used, establishing how the healthcare provider will be involved, and robust patient education to support understanding the technology, how it works, how to troubleshoot, and where to access help.
Similarly, not only can the data collected from a digital health technology be used to monitor patient outcomes and inform understanding whether a treatment is effective, but it can also support prevention, intervention, and remediation strategies. For example, daily monitoring of metrics such as the availability of patient-specific data, device charge state, and location (i.e., GPS) can be used as objective measures of patient adherence to the technology, enabling more rapid interventions to be developed and implemented. Most importantly, when patients are not using the digital tool as intended, it's essential to identify this inconsistency and execute a targeted intervention plan as quickly as possible and re-engage them.
Broadening the impact of real-world data
Deploying a strategic framework also provides a roadmap to further understanding the complex interactions between patients, digital technology, and the many secondary effects of those interactions. The cumulative effects of these interactions have broad implications for patient well-being, as they can help motivate patients to adhere to — or improve adherence with — their treatment plans and medical advice.
As an example, an app that provides behavioral therapy to mental health patients may not only facilitate their access to cognitive therapy, but their use of the app may also correlate to adherence with their medications and in turn incentivize them to use the app more. Secondary effects, such as improved family and social relationships, more frequent interactions with their doctors, and greater community involvement, can also provide data-driven insights to create better patient experiences with personal, measurable, and direct solutions.
What Can We Help You Solve?
Exponent is at the forefront of rapid developments in digital health technology. We can support you in developing innovative solutions and large-scale deployment and adoption. Our scientists across multiple disciplines are uniquely equipped to help identify challenges and opportunities in understanding, evaluating, and optimizing patient adherence.

Biomechanical Expertise for Wearables
Leverage wearables to unlock value in healthcare and enhance personalized patient outcomes.

Biosensor Integration & Biosignal Processing for UX Research
Leverage valuable psychophysiological and biosignal user data to enhance product design.

Improve User Research & Testing
Human factors investigations for data-driven product and process design decisions.

Next-Gen Wearables in Healthcare
Effectively demonstrate the clinical, experiential, and economic value of wearable devices.

Real-World Evidence Consulting
Leverage real-world data to improve healthcare decisions.




